Periodontal disease silently affects nearly half of all American adults over 30, often progressing without obvious symptoms until significant damage has occurred. The condition begins as inflamed gums but can advance to destroy the bone and tissue supporting your teeth, ultimately leading to tooth loss if left untreated. Understanding your treatment options and seeking timely care can make the difference between preserving your natural smile and facing extensive dental restoration.
Periodontal care encompasses various treatments designed to stop disease progression, restore gum health, and help you maintain your natural teeth. At Dental Group of Chicago, we provide comprehensive periodontal disease treatment with flexible hours to accommodate busy schedules, making quality care accessible when you need it most.
Understanding Periodontal Disease
Periodontal disease develops when bacterial plaque accumulates along and beneath the gum line, triggering an inflammatory response. Gingivitis represents the first stage, caused by plaque buildup along the gum line. In this initial stage, your gums become inflamed, appear red and swollen, and may bleed during brushing or flossing. While gingivitis can often be reversed with improved oral hygiene and professional cleanings, untreated cases progress to periodontitis.
As periodontitis develops, inflammation extends deeper into the supporting structures of your teeth. Gums pull away from tooth surfaces, forming pockets where bacteria accumulate and multiply. These infected pockets trigger your body’s immune response, which, combined with bacterial toxins, begins breaking down the bone and connective tissue holding your teeth in place. Chronic periodontitis affects 47.2% of adults over 30 in the United States and can lead to the loss of tissue and bone supporting your teeth. This destruction occurs progressively, and advanced cases result in loose teeth or tooth loss.
Treatment Options for Periodontal Disease
Treatment approaches vary based on disease severity, your overall health, and how well you’ve responded to earlier treatments. Our team evaluates each case thoroughly to determine the most appropriate interventions for your situation.
Scaling and Root Planing
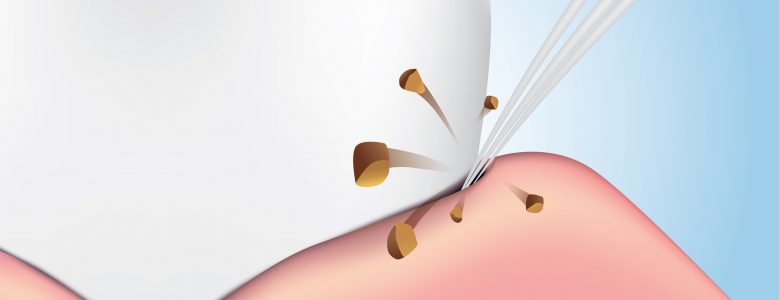
This deep cleaning procedure serves as the foundation of periodontal disease treatment for most patients. Scaling removes plaque and tartar from tooth roots, while root planing smooths the root surfaces so gum tissue can reattach. The procedure involves cleaning below the gum line to remove bacterial deposits and hardened tartar from tooth roots.
During scaling, we use instruments to carefully remove plaque and tartar from both above and below the gum line. Root planing then smooths the root surfaces, removing bacterial toxins and creating a clean surface where gum tissue can reattach to your teeth. This smoothing also makes it more difficult for bacteria to recolonize the area. Most patients receive local anesthesia during this treatment to ensure comfort throughout the procedure.
Depending on the extent of your periodontal disease, we may treat one section of your mouth per appointment or address all affected areas in fewer, longer sessions. Following treatment, you may experience some sensitivity and mild discomfort for a few days, but these symptoms typically resolve quickly as your gums begin healing.
Antibiotic Therapy
Some cases benefit from antibiotic therapy used alongside mechanical cleaning treatments. We may recommend local antibiotics placed directly into periodontal pockets after scaling and root planing. These controlled-release medications slowly dissolve over several days, delivering concentrated antibacterial effects right where infection exists.
Systemic antibiotics in pill or capsule form may be prescribed for more widespread or aggressive infections. These medications work throughout your body to help control bacterial infection and support the healing process, particularly when combined with professional cleaning procedures.
Surgical Treatments
When non-surgical approaches don’t sufficiently reduce pocket depths or stop disease progression, surgical interventions may become necessary to preserve your teeth. Several surgical options address different aspects of periodontal disease and its effects on your oral structures.
Flap surgery involves lifting back the gums to provide direct access to tooth roots and underlying bone. After thoroughly cleaning the roots and removing diseased tissue, we reposition the gum tissue to fit snugly around your teeth, reducing pocket depth and making it easier for you to keep the area clean through daily home care.
Bone grafting procedures help rebuild bone destroyed by periodontitis. We place grafting material in areas of bone loss to encourage natural bone regeneration, providing stronger support for your teeth. Similarly, soft tissue grafting addresses gum recession by taking tissue from your palate or another source and attaching it to areas where gums have pulled away from teeth.
Long-Term Maintenance and Prevention
Successfully treating periodontal disease requires ongoing commitment to oral health beyond the initial treatment phase. Most patients require periodontal maintenance cleanings every three to four months following active treatment, as these more frequent visits help prevent disease recurrence and catch any problems early. Your daily care routine remains essential to long-term success. Consider these key practices for maintaining healthy gums after treatment:
- Brush twice daily with a soft-bristle toothbrush using proper technique
- Floss once daily to remove plaque from between teeth and below the gum line
- Use an antimicrobial mouthrinse formulated to reduce bacteria associated with gum disease
- Avoid tobacco products, as smoking significantly increases recurrence risk
- Manage systemic health conditions, particularly diabetes, through proper medical care
- Maintain a balanced diet rich in nutrients to support immune function and tissue health
These practices work together to keep your gums healthy and prevent the return of periodontal disease.
Lifestyle modifications provide important support for gum health. If you smoke, quitting significantly improves treatment outcomes and reduces your risk of disease recurrence. Managing systemic conditions, particularly diabetes, helps keep periodontal disease under control. Stress reduction techniques and maintaining proper nutrition support immune function and tissue health, contributing to better periodontal outcomes. Our team can provide guidance on general dentistry practices to maintain your oral health between periodontal maintenance visits.
Periodontal Disease Treatment at Dental Group of Chicago
Our team combines clinical experience with a commitment to accessible, patient-centered care. We’re open Monday through Friday from 8 AM to 8 PM and Saturdays from 8 AM to 2 PM, offering flexibility for patients with demanding schedules. Our South Loop location at 1035 S Michigan Ave provides convenient access to quality periodontal care for patients throughout the greater Chicagoland area. We accept most major insurance plans, including Delta Dental, MetLife, Cigna, BlueCross BlueShield, Guardian, and United Healthcare.
If you notice signs of gum disease, such as bleeding gums, persistent bad breath, gum recession, or loose teeth, don’t wait to seek care. Early intervention leads to better outcomes and often requires less extensive treatment. Even without obvious symptoms, regular dental examinations can detect periodontal disease in its early stages when treatment is simpler and more successful. Our dental team brings extensive training in periodontal care and stays current with the latest treatment approaches while maintaining our focus on preserving your natural teeth whenever possible. Contact us today to schedule a comprehensive periodontal evaluation and take the first step toward healthier gums.